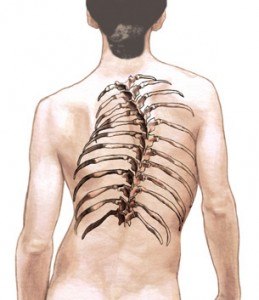
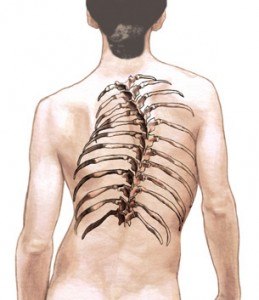
Scoliosis
Sometimes scoliosis Treatments requires spine surgery. The goal of surgery is to stop the scoliotic curve(s) from progressing (growing larger), manage deformity, and stabilize the spine. Scoliosis surgery involves spinal fusion with instrumentation.
About scoliosis
Scoliosis is an abnormal side-to-side spinal curve that develops in the thoracic (mid back) and/or lumbar (low back) spine. Scoliosis can develop at any age. It can be classified as:
- Congenital (at birth)
- Infantile (age 3 or younger)
- Juvenile (ages 4 to 10 years)
- Adolescent (ages 10 to 18)
- Adult (Over age 18)
Pre-surgical considerations
As stated, the goals of scoliosis surgery include: stop the curve(s) from progressing in size, manage deformity, and stabilize the spine. The type of surgery your neurosurgeon recommends is based on many factors, including your chronological age, type and cause of scoliosis, curve size, curve location(s), existing deformity, and its potential to progress. Your neurosurgeon carefully considers all the information collected during your physical and neurological examinations, diagnostic testing, pain and symptoms, and co-existing medical problems (i.e., diabetes, endocrine dysfunction, bone disease).
About scoliosis spine surgery
Scoliosis surgery is performed under general anesthesia. It is usually performed from the front, back, or both front and back sides of your body: anterior, posterior, anterior-posterior.
- Anterior approach: the surgery is performed through either the abdomen and/or one or both sides of the chest wall. The patient is positioned face down or either on their left or right side. Reaching the spine anteriorly through the chest wall involves deflating a lung and removing a rib. The lung is re-inflated during surgery. The rib bone is a source of autograft; the patient’s own bone that can be prepared into bone graft.
- Posterior approach: the surgery is performed through the back (rear) of the spine. The size of the incision depends on the location, size and number of curves (spinal levels) to be treated. The patient is positioned face down on the operating table.
- Although scoliosis surgery is considered complex, an anterior-posterior approach is the most challenging for the patient and neurosurgeon. The dates of the front and back surgeries may be staggered; in other words, not performed on the same day.
You (or your child) may be a candidate for minimally invasive spine surgery (MISS). There are different ways the surgery can be performed, and your neurosurgeon explains the possible benefits and risks associated with his surgical recommendations. Your neurosurgeon may use a sophisticated image guided technology to pre-plan the surgery days in advance and use it during scoliosis surgery.
Scoliosis surgery often involves removal of one or more intervertebral discs (discectomy) and/or bone (i.e., vertebral body, spinous process). Spinal instrumentation, such as rods and screws, permanently fix the spine in a more normal position and provide immediate stabilization of the spine. Bone graft (spinal fusion) is packed between bony voids and around the instrumentation. The purpose of bone graft is to stimulate bone to heal—fuse solid.
Surgery can last several hours. Post-operative bracing may not be required. The average hospital stay is a week, although much depends on your scoliosis and the type of surgery recommended.
Before your procedure
Well in advance of your surgery day, your neurosurgeon explains how he performs your procedure. During the discussion, you learn if your procedure can be performed as a minimally invasive spine surgery or open approach, and why.
Before surgery, you visit your primary care doctor and/or other medical specialists (i.e., heart doctor, endocrinologist) to obtain a general health clearance. This means your doctor has carefully evaluated your health in terms of undergoing surgery. Your assessment may include blood tests, x-rays or other imaging studies, as well as special tests for existing medical problems (i.e., cardiopulmonary disease, diabetes).
Review potential benefits and risks
Of course, the potential benefits of the surgery are important to know, but so are the possible risks and complications. Your risks and complications may be different from those of another patient because you are unique. Your neurosurgeon takes that into serious consideration and thoughtfully explains potential risks to you, which may include infection, bleeding, reaction to anesthesia, and nerve damage.
After surgery
You are moved from the operating room into the recovery area. Here, the nurses and medical staff closely monitor your vital signs with attention to managing post-operative pain. You should expect some discomfort.
Post-operative care
Your surgery is over, but now your recovery starts! If you do not understand your post-surgical instructions or a problem develops, please call us—we are here to help you.
Conventional post-spine surgery instructions include:
- Schedule your post-operative appointment (call 281.446.3876).
- Keep your incision(s) dry and clean.
- You may shower, but keep your incision(s) covered and dry.
- Rest; you will fatigue easily while your body heals.
- Do not take a tub bath, go swimming, or sit in a hot tub or pool.
- Begin physical therapy and/or exercise as instructed.
- Take medications as prescribed.
- Do not lift or carry anything heavier than a shoe.
- Walking is encouraged.
- Do not drive until cleared by your neurosurgeon.
- Avoid riding in a car; short distances are permitted.
- Do not smoke or use tobacco.
- Eat well, your body needs nutritious food to heal.
Call your neurosurgeon's office (281.446.3876)
- Fever 101 degrees Fahrenheit or higher.
- Redness and/or swelling around the incision site expands.
- Change in the amount, odor or appearance of the incision drainage.
- Incision pain increases.
- Bowel or bladder dysfunction develops.
- Genital area numbness develops.
Talk with your neurosurgeon
We hope this information about scoliosis surgery has answered your immediate questions. Remember, your neurosurgeon is your most valuable source to answer your questions about symptoms, Treatments and your healthcare. |